Functional Genomics in Healthcare
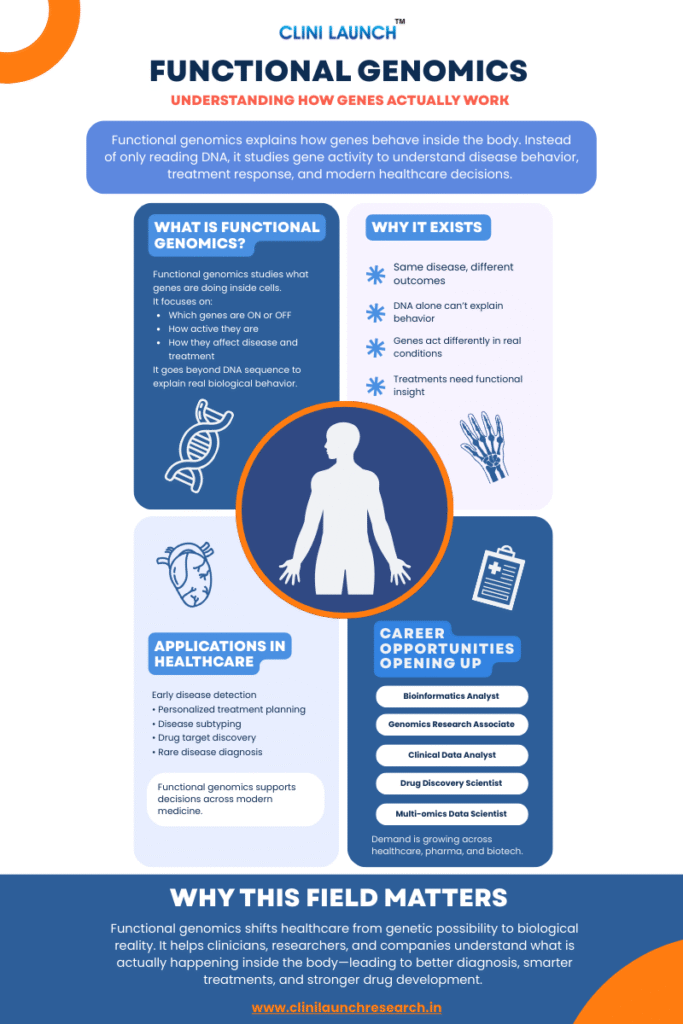
Functional genomics in healthcare exists because knowing what is written in DNA is no longer enough to understand how diseases behave in real patients. People with the same diagnosis and similar genetic reports often experience very different symptoms, disease progression, and treatment outcomes.
Traditional genetic testing identifies DNA variations, but it often cannot explain how those genes behave inside the body or why outcomes vary so widely. Clinical resources such as MedlinePlus from the U.S. National Library of Medicine highlight this limitation, which pushed healthcare toward approaches that study gene activity, biological pathways, and molecular behavior instead of DNA sequence alone.
This blog introduces what functional genomics is, why it became necessary in modern healthcare, and how it is applied today through real-world examples.
| Functional genomics in healthcare studies how genes and their products (RNA and proteins) function in the body to explain disease behavior and treatment response. Instead of focusing only on DNA sequences, it analyzes gene expression, molecular pathways, and biological activity to improve diagnosis, therapy selection, and understanding of disease progression. |
What Is Functional Genomics?
Functional genomics is the study of how genes function inside the body, not just what their DNA sequence looks like. Instead of focusing only on which genes are present, it examines how genes behave, when they are active, and how they influence biological processes in real conditions.
Genes are constantly being switched ON and OFF. Some activate only during illness or stress, while others remain silent. Functional genomics focuses on gene expression analysis to understand what is actually happening inside cells as diseases develop or respond to treatment.
Traditional Genomics vs Functional Genomics
Traditional genomics provides static information about DNA, which rarely changes. Functional genomics captures dynamic biological activity, showing how genes interact with proteins, pathways, and cellular systems over time.
In simple terms, traditional genomics tells us what could happen, while functional genomics explains what is happening right now. This distinction is critical for understanding complex diseases.
Case Study: Rheumatoid Arthritis and the Limits of Genetic Risk
| Aspect | Details |
|---|---|
| The Problem | Thousands of genetic variants are linked to rheumatoid arthritis, yet many patients do not respond to treatment. |
| What Functional Genomics Revealed | Analysis of DNA folding and gene regulation in immune cells identified which genes were actually affected. |
| What Changed | New disease-driving pathways were identified that required activation rather than inhibition. |
| Why This Matters | Functional genomics transformed genetic associations into actionable biology. |
What Functional Genomics Is NOT
- Not just DNA sequencing: It focuses on gene activity, not only DNA reading.
- Not a single test: It combines multiple biological datasets.
- Not limited to cancer: Used in autoimmune, neurological, metabolic, and rare diseases.
- Not a replacement for clinicians: It supports medical decisions, not replaces them.
- Not only experimental: Already used in diagnostics and treatment planning.
Modern healthcare reached a point where genetic information alone stopped being sufficient. DNA sequencing can identify mutations, but it often fails to explain disease behavior or treatment outcomes.
Diseases such as cancer and autoimmune disorders involve networks of genes and pathways that change over time. Functional genomics addresses this by focusing on gene activity rather than genetic potential.
Functional genomics is actively used in pharmaceutical research. Companies like AstraZeneca apply it to link genetic data with biological function and improve drug discovery outcomes.
| Aspect | Details |
|---|---|
| The Problem | Cancer drug development fails frequently and late in trials. |
| What Functional Genomics Revealed | CRISPR screening identified genes cancers truly depend on. |
| What Changed | Drug targets could be prioritized with higher success probability. |
| Why This Matters | Functional genomics reduces wasted effort in drug discovery. |
Bioinformatics and Metabolomics
Build real-world skills in bioinformatics and metabolomics used across healthcare, pharma, and life sciences. Learn to analyze multi-omics data, identify biomarkers, and translate complex biological data into actionable insights using modern analytical pipelines.

Duration: 3 months
Skills you’ll build:
Applications of Functional Genomics in Healthcare
Functional genomics is applied wherever understanding biological activity matters more than simply knowing which genes exist. In healthcare, this shift has transformed how diseases are detected, classified, treated, and studied over time.
Many diseases begin with molecular changes long before symptoms appear. Functional genomics helps detect these early signals by identifying abnormal patterns of gene activity and pathway disruption.
In cancers, altered gene expression can signal tumor development before it becomes visible on scans. In neurological conditions such as Alzheimer’s or Parkinson’s disease, early disruptions in neuronal signaling and metabolic pathways can be detected years before clinical diagnosis.
By detecting abnormal gene activity before symptoms appear, functional genomics strengthens molecular diagnostics and enables earlier, more accurate intervention.
| Aspect | Details |
|---|---|
| The Problem | Gastric cancer is highly resistant to chemotherapy, and many drug combinations fail despite targeting known pathways. |
| What Functional Genomics Revealed | Screening revealed that a drug combination worked because one drug blocked the cancer cell’s drug-efflux mechanism. |
| What Changed Because of It | Researchers understood why the combination worked and identified patients most likely to benefit. |
| Why This Case Matters | Functional genomics revealed what drugs were actually doing inside cells. |
Patients with the same diagnosis often respond differently to the same treatment. Functional genomics explains this by revealing how active disease-related pathways are in individual patients.
In oncology, functional profiling identifies whether tumors are driven by growth signaling, immune evasion, or metabolic changes. In autoimmune diseases, it distinguishes inflammatory patterns that appear similar clinically but require different therapies.
By aligning treatment choices with biological behavior rather than labels, functional genomics reduces trial-and-error medicine.
Many diseases that appear identical under standard testing are biologically different at the molecular level. Functional genomics enables disease subtyping based on gene activity rather than symptoms alone.
This is especially important in cancers, blood disorders, and neurological diseases, where molecular subtypes predict aggressiveness, recurrence risk, and long-term outcomes.
Targeting the wrong biological signal leads to failed therapies. Functional genomics helps identify which genes and pathways are actually driving disease.
By studying gene activity and pathway behavior, researchers validate whether targets play a causal role in disease progression. This improves target selection and reduces late-stage drug failures.
Rare genetic disorders often remain unexplained even after DNA sequencing. Functional genomics bridges this gap by showing how genetic changes disrupt biological pathways.
In inherited metabolic disorders, neuromuscular diseases, and rare epileptic syndromes, functional analysis clarifies whether a variant is harmful and how it affects the body.
Functional genomics predicts how patients respond to therapies by studying gene activity linked to drug metabolism, signaling pathways, and resistance mechanisms.
In cancer treatment, it explains why resistance develops and guides alternative strategies before disease progression worsens.
| Aspect | Details |
|---|---|
| The Problem | Many rare disease patients remain undiagnosed even after DNA sequencing. |
| What Functional Genomics Revealed | RNA sequencing showed how variants affected gene expression and splicing. |
| What Changed Because of It | Diagnostic accuracy improved for patients with no prior answers. |
| Why This Case Matters | Functional genomics turns uncertain genetic data into diagnoses. |
Functional genomics is used to track how diseases evolve over time. Changes in gene expression can indicate whether a disease is progressing, stabilizing, or responding to therapy.
This allows clinicians to adjust treatment plans based on biological response rather than waiting for symptoms or imaging changes.
| Functional genomics is increasingly used for continuous monitoring by tracking changes in biological activity over time. This supports dynamic care decisions based on molecular response rather than delayed clinical signs. |
Functional genomics aligns with systems biology by integrating gene activity with broader biological networks. Instead of viewing genes in isolation, it models how genes, proteins, and pathways interact within the body.
This systems-level understanding supports more comprehensive disease models and improves how complex conditions are diagnosed and managed across healthcare settings.
Functional genomics has reshaped how healthcare understands disease. Instead of relying only on DNA sequences, it focuses on how genes behave in real biological conditions, helping explain differences in disease progression, treatment response, and clinical outcomes.
As medicine becomes more personalized and data-driven, understanding gene activity and biological pathways is no longer optional across healthcare and life sciences. Functional genomics now sits at the core of modern diagnosis, research, and drug development.
From a career perspective, this shift has created growing demand for professionals who can interpret functional genomic data in clinical research, molecular diagnostics, bioinformatics, and precision medicine roles.
At CliniLaunch, we help learners build this foundation through healthcare and life sciences programs aligned with real-world clinical and research needs. Functional genomics is not just an emerging concept—it reflects how modern medicine now approaches disease, through function rather than sequence.
Frequently Asked Questions (FAQs)
Functional genomics informs how diseases are classified, which diagnostic tests are ordered, and how treatments are prioritized by revealing pathway activity and gene expression patterns rather than relying only on DNA variants.
It supports oncologists, neurologists, and immunologists in choosing therapies that align with a patient’s real-time disease biology instead of static genetic risk alone.
Functional genomics enhances molecular diagnostics by detecting abnormal gene expression and pathway disruptions before symptoms or imaging changes appear.
This enables earlier risk assessment, more accurate disease classification, and improved use of tools such as RNA-seq–based panels and multi-omics signatures in cancer, neurological, and autoimmune conditions.
In drug discovery, functional genomics confirms which genes and pathways actually drive disease, reducing the risk of pursuing non-causal targets.
It also accelerates biomarker discovery by linking gene activity patterns with treatment response, resistance, and disease progression, leading to more efficient and better-stratified clinical trials.
Emerging roles include bioinformatics analyst, multi-omics data scientist, clinical genomics researcher, and molecular diagnostics specialist.
Professionals in these roles require skills in genomic data analysis, systems biology, biomarker discovery, and AI-enabled interpretation of high-throughput biological data to translate functional genomics into clinical and pharmaceutical decisions.
AI and data science are used to analyze large functional genomics datasets, identify complex gene expression patterns, and predict treatment response or resistance.
These approaches integrate genomics, transcriptomics, proteomics, and metabolomics into practical tools for precision medicine, clinical research, and hospital-level decision support by automating variant interpretation, risk prediction, and drug response modeling.





