Today, R programming in healthcare has become a foundational skill for analyzing complex medical data, supporting clinical research, and enabling evidence-based decisions. From hospitals to research labs, R programming in healthcare is increasingly used to turn raw data into reliable insights that improve patient outcomes.
When it comes to analyzing medical data, visualizing gene activity, or predicting trends, R programming is one of the most powerful tools available in healthcare today. R isn’t just about basic statistics it’s about unlocking insights from vast datasets with ease.
With a vast library of statistical functions and specialized healthcare tools, R empowers healthcare professionals to perform advanced analysis, generate meaningful visualizations, and uncover patterns that drive decisions.
A widely cited 2015 survey by Rexer Analytics found that 76% of analytics professionals use R. Its ability to handle massive datasets and make evidence-based predictions has made it the go-to tool for transforming raw data into actionable insights. This growing adoption highlights the importance of R programming for modern healthcare professionals who must work with large, complex, and sensitive medical datasets.
Mastering R is essential for healthcare professionals to make data-driven decisions in clinical research, patient care, and biotechnology. Now, let’s explore how R programming is impacting various healthcare areas, from gene analysis to personalized medicine.
| Featured Snippet: R programming in healthcare helps professionals analyze clinical data, study disease trends, and support research in genomics, trials, and public health. It is widely used in hospitals, pharma, and research labs for data-driven healthcare decisions. |
What Is R Programming in Healthcare?
R programming in healthcare refers to using the R language to analyze and interpret medical, clinical, and biological data. It is widely used in hospitals, research labs, pharma, and public health to work with patient data, clinical trials, and large biomedical datasets.
R is built specifically for statistics and data analysis, making it ideal for tasks like hypothesis testing, outcome analysis, predictive modeling, and data visualization. Its reliability and reproducibility make it a trusted tool for clinical research, regulatory work, and evidence-based healthcare decisions.
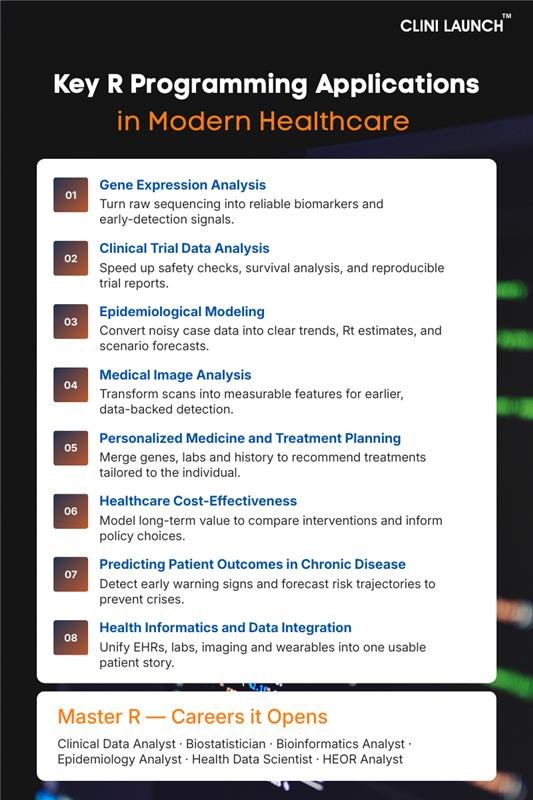
Applications of R Programming in Healthcare – How R Programming is Transforming Key Areas of Healthcare and Life Sciences
1 .Gene Expression Analysis
Gene expression analysis looks at which genes are “turned on” or “turned off” in a cell or tissue. Imagine each gene as a factory line producing a product (a protein). Gene expression measures how much product each line is making right now. In experiments, scientists compare two states, for example, tumour vs normal tissue, to find which factory lines are working harder or quieter. The end goal is to find a small list of genes whose changed activity explains the biological difference you care about.
Situation before R Programming
Before R became common, researchers handled gene expression with a messy mix of spreadsheets, separate tools, and manual steps. Labs produced raw output from sequencers or microarrays, but turning that into a clean table ready for analysis needed a lot of custom work. Different labs used different methods, so results didn’t always match. People often used one tool for normalization, another for statistics, and another for plotting — moving data between programs by hand. That made the work slow, error-prone, and hard to reproduce. If someone asked “how did you get this result?” there was often no single clear answer.
What changed after integrating R Programming in Gene Expression Analysis
R brought everything into one place: cleaning the data, correcting technical differences between runs, doing the right statistics for count-based gene data, drawing clear figures, and making a single reproducible report. Specialized R packages were created by genomics researchers for genomics problems, so common tasks like normalizing read counts or testing thousands of genes at once became straightforward and statistically sound. Instead of juggling files and tools, scientists could write one script that read the raw data, ran the analysis, and produced the figures and written report and anyone else could run the same script and get the same results. That made experiments faster, more reliable, and easier to trust.
Why this matters?
For students, this is practical: learning R means you can move from raw biological data to trustworthy conclusions. If you want to work in a lab, biotech, hospital research, or drug discovery, employers expect you to be able to clean data, check if results are real or noise, and create clear plots and reports that clinicians and researchers can rely on. Knowing the R workflow also teaches you good scientific habits, reproducibility, transparent methods, and careful statistical thinking, which are valued across research and clinical teams. In short, R turns pile-of-files biology into reproducible evidence you can act on.
R Programming Tools Used in Gene Expression Analysis:
| Process Stage | R Tools / Packages | What the Tools Do |
|---|---|---|
| Data Cleaning & Preparation | dplyr, tidyr, data.table | • Clean and filter gene tables • Handle missing values & inconsistent formats • Reshape data (wide ↔ long) • Process large RNA-seq matrices fast |
| Differential Expression Analysis | DESeq2, edgeR, limma | • Identify up/down-regulated genes • Normalize gene counts • Compute fold changes & p-values • Compare disease vs control groups |
| Visualization & Pattern Detection | ggplot2, ComplexHeatmap, EnhancedVolcano, PCAtools | • Create PCA plots & clustering visuals • Generate heatmaps for expression patterns • Build volcano plots for DE genes • Visualize sample similarities/differences |
| Biological Interpretation | clusterProfiler, ReactomePA, gProfileR | • Perform pathway enrichment (KEGG/GO) • Link genes to biological mechanisms • Identify disease-related pathways • Discover functional gene groups |
| Reporting & Output | R Markdown, knitr, Shiny | • Create reproducible analysis reports • Generate formatted tables & visuals • Build interactive dashboards • Share results with researchers/clinicians |
| Case Insight: Colorectal Cancer Research Using R In a recent study on colorectal cancer, researchers analyzed RNA-Seq data from cancerous and healthy tissues to find genes that could serve as biomarkers for early detection. Using R, they processed the data and identified 1,641 differentially expressed genes that played key roles in various signaling pathways. Among these, genes like MMP7, TCF21, and VEGFD stood out as promising candidates for diagnosing colorectal cancer. By pinpointing these biomarkers, the study opens the door to earlier detection methods, which could significantly improve patient outcomes. Early diagnosis in cancer is crucial, and this R-powered analysis brings us one step closer to better, more accurate diagnostic tools. |
In short, R programming in healthcare turns complex biological data into reproducible evidence that researchers and clinicians can trust.
2. Clinical Trial Data Analysis
Clinical trial data analysis is the process of checking whether a new drug or treatment actually works and whether it is safe. Every patient in a trial generates information, symptoms, lab values, side effects, responses to treatment, and this information needs to be combined and studied carefully. The goal is to compare groups (such as the drug group vs the placebo group) to see if the treatment truly makes a meaningful difference and if any safety concerns appear early. In simple terms, this analysis turns patient records into scientific evidence.
Before R (how teams handled trial data earlier)
Before R became common, trial data was handled through a combination of spreadsheets, manual cleaning, and rigid software like SAS. Much of the work involved fixing errors by hand, adjusting formats, merging patient files, and double-checking details, a slow and repetitive process. Visualizing patterns, such as survival trends or side-effect timelines, often required separate tools or manual charting. Updates were painful: if even one patient’s data changed, analysts had to redo entire parts of the analysis manually. This made the process slow, error-prone, and difficult to reproduce in a transparent way.
How the workflow changed after integrating R Programming in Clinical Research and Trials
R brought flexibility, speed, and transparency into trial analysis. Instead of working with multiple disconnected tools, analysts could clean the data, run statistical tests, create survival curves, compare treatment arms, and generate full reports all within one environment. R automated much of the repetitive work, so when new patient data arrived, the entire analysis, figures, tables, and summaries, could update instantly. It also made results easier to reproduce and share, which is essential in clinical research where every number must be traceable. For modern trials that generate large and complex datasets, R made analysis faster, clearer, and scientifically stronger.
Why this matters to life science and healthcare students
If you want to work in clinical research, pharmacovigilance, or healthcare analytics, you will eventually work with trial data. Understanding how to clean datasets, compare patient outcomes, look for safety patterns, and create simple but meaningful visual summaries is a core skill in this field. R helps you learn these skills in a way that aligns with real industry workflows. It also builds the foundation for roles in CROs, pharma companies, hospitals, and regulatory teams, where the ability to work confidently with trial data is a major advantage. In other words, learning R helps you move from “reading clinical studies” to contributing to them.
R Programming Tools Used in Clinical Trial Data Analysis:
| Process Stage | R Tools / Packages | What the Tools Do |
|---|---|---|
| Data Cleaning & Preparation | dplyr, tidyr, data.table | • Organize patient datasets into structured formats |
| Statistical Analysis | survival, survminer, stats, lme4 | • Estimate treatment effects with survival models • Compute hazard ratios using Cox models • Analyze longitudinal data with mixed-effects models • Perform hypothesis testing for study endpoints |
| Visualization & Safety Monitoring | ggplot2, survminer, plotly | • Plot survival curves and event timelines • Visualize dose–response and treatment differences • Create dynamic safety charts for AE patterns • Build interactive visual reviews (plotly dashboards) |
| Reporting & Regulatory Output | R Markdown, knitr, Shiny | • Generate submission-ready clinical summaries • Automate TLFs (Tables, Listings, Figures) • Build interactive dashboards for safety/efficacy review • Compile reproducible reports for FDA/EMA audits |
Many of these workflows rely on specialized R packages for clinical trials that support survival analysis, safety monitoring, and regulatory reporting.
| Case Insight: Analyzing Clinical Trial Data for New Drug Development In a study analyzing clinical trial data for a new cancer drug, researchers used R to evaluate survival rates and side effects in patients. By applying survival analysis techniques such as the Kaplan-Meier estimator and Cox Proportional Hazards model, they gained valuable insights into how the drug performed over time. Visualizations created using ggplot2 helped stakeholders quickly interpret the data, leading to more informed regulatory discussions. The findings, powered by R, not only contributed to the regulatory approval of the drug but also highlighted potential areas for future research, making it a crucial part of the drug development process. |
Clinical Research
Build industry-ready skills for clinical trials, regulatory compliance, and drug safety. This program prepares you to work across clinical operations, data management, pharmacovigilance, and regulatory workflows in healthcare and pharma.

Duration: 12 months
Skills you’ll build:
3. Epidemiological Modeling
Epidemiology is all about understanding how diseases move through a population, who gets infected, how fast it spreads, and what might happen next. During any outbreak, health agencies collect huge amounts of data every day: new cases, tests, deaths, recoveries, and vaccination numbers. But this data almost never arrives clean or consistent. Some places report late, some miss days, and numbers often jump because of festivals, policy changes, or sudden increases in testing.
The challenge before R
Before tools like R were used, epidemiologists relied on spreadsheets and manual calculations to understand what was happening. The problem was simple: daily disease data is noisy and unstable.
Numbers rise one day, fall the next, and often don’t reflect real trends. Because of this, it was extremely difficult to answer basic questions quickly:
- Are cases genuinely rising or is it just a reporting delay?
- Is the infection slowing down?
- Is vaccination making an impact?
- Should hospitals prepare for a surge?
This meant decisions were often slower and less confident than they needed to be.
What changed after integrating R Programming in Epidemiology and Public Health
R made epidemiology faster, clearer, and far more responsive.
Instead of struggling with scattered data, R allows analysts to:
- clean and organize daily case numbers into proper timelines,
- smooth the noise so true trends become visible,
- estimate how quickly the disease is spreading,
- forecast short-term surges or declines,
- and visualize everything through simple, readable graphs.
This ability to turn noisy outbreak data into actionable insights demonstrates the strength of R programming epidemiology in real-world public health decision-making
| The biggest advantage? R turns unpredictable, messy outbreak data into something that public-health teams can act on immediately. Hospitals can plan beds, governments can prepare guidelines, and vaccination teams can target the right regions, all because R helps reveal the real pattern behind the confusion. |
Why this matters?
Whether you’re studying microbiology, biotechnology, public health, or clinical research, epidemiology is a part of your world. Being able to understand disease patterns is not just useful, it’s becoming a core skill.
Learning R gives you the ability to:
- interpret real outbreak data instead of just memorizing theory,
- support real-world decisions during public-health crises,
- collaborate with epidemiologists, clinicians, and data teams,
- and move into careers involving disease surveillance, public health, and healthcare analytics.
R Programming Tools Used in Epidemiological Modeling
| Process Stage | R Tools / Packages | What the Tools Do |
|---|---|---|
| Data Cleaning & Preparation | dplyr, tidyr, data.table | Organize daily case counts into proper time-series • Fix inconsistent date formats and regional codes • Merge multiple surveillance datasets (district, state, national) • Handle missing or delayed case reporting |
| Exploratory Trend Analysis | ggplot2, zoo, TTR | • Calculate moving averages and highlight trend shifts • Plot epidemic growth curves and positivity-rate trends • Smooth noisy data to reveal real outbreak patterns |
| Mathematical Modeling & Forecasting | EpiEstim, epitools, epidemia, forecast | • Estimate reproduction numbers (R₀, Rt) from real-time data • Fit SIR/SEIR models to simulate disease behavior • Generate short-term and long-term outbreak forecasts • Evaluate intervention impact (lockdowns, vaccination boosts) |
| Model Validation | tidymodels, yardstick | • Compare predicted vs. observed case trends • Measure forecast accuracy using epidemiology metrics • Perform sensitivity tests to see how assumptions affect model results |
| Visualization & Dashboards | plotly, leaflet, shiny | • Build interactive epidemic dashboards • Display geospatial spread on dynamic maps • Enable real-time exploration of transmission patterns |
| Reporting & Communication | R Markdown, knitr | • Generate epidemiology situation reports (daily/weekly) • Combine forecasts, maps, and trend charts into polished documents • Automate public-health reporting workflows |
| Case Insight: Modeling COVID-19 Spread Using R During the COVID-19 pandemic, R was instrumental in modeling the spread of the virus. Researchers used R to calculate reproduction numbers (R0) and assess the effectiveness of interventions like lockdowns and vaccination campaigns. This modeling helped predict the future trajectory of the disease, giving governments vital information to manage healthcare resources and implement timely interventions. R’s role in predicting and controlling the spread of COVID-19 demonstrates its power in public health. By enabling data-driven decision-making, R helped shape the global response, ensuring better outcomes for individuals and communities during a time of crisis. |
Biostatistics
Build strong statistical foundations for healthcare, clinical research, and life sciences. This program trains you to design studies, analyze biomedical data, apply statistical tests, and interpret results for real research and industry work.

Duration: 12 months
Skills you’ll build:
Other Courses
4. Medical Image Analysis
Medical scans look simple on the surface, but anyone who has worked with MRI or CT images knows they’re far from regular pictures. Each scan contains layers of technical information, differences from machine to machine, and subtle patterns that aren’t obvious to the naked eye. For healthcare, the challenge isn’t getting the image, it’s understanding what the image really means.
Before R: When Imaging Relied Almost Entirely on the Human Eye
For years, radiologists examined scans manually, slice by slice. It worked, but it had real limitations:
- tiny lesions were easy to miss,
- images from different hospitals didn’t behave the same way,
- measuring tumors or abnormalities took a huge amount of time,
- and quantitative analysis (actual numbers) was nearly impossible without specialized, expensive software.
Imaging was powerful, but the analysis depended too heavily on visual judgment, which limited how deep researchers could go.
After R Programming in Medical Imaging: Turning Scans Into Meaningful, Measurable Insight
R changed imaging by giving researchers a way to treat every image like structured data instead of a flat picture.
With R, teams can now:
- clean and standardize scans so they are comparable,
- extract features like size, texture, density, or thickness,
- highlight subtle abnormalities that the eye might overlook,
- analyze how a tumor or tissue changes over time,
- and produce clear, traceable visual overlays that support diagnosis.
This shift moved imaging from “interpretation” toward evidence-backed measurement, which is crucial for modern clinical research.
Why This Matters for Life Science and Healthcare Students
Whether you plan to work in pharma, clinical research, biotechnology, neuroscience, or diagnostics, imaging is becoming central to the future of healthcare.
Understanding how R works with images helps you:
- see the deeper biological meaning hidden inside MRI/CT data,
- collaborate confidently with radiology teams during trials,
- engage in radiomics and AI-driven imaging careers,
- and understand disease progression through data, not just visuals.
Medical imaging is no longer just about looking, it’s about analyzing, quantifying, and learning from what the scan contains. Mastering R programming in healthcare gives you that ability to bridge this gap.
R Programming Tools Used in Medical Image Analysis:
| Process Stage | R Tools / Packages | What the Tools Do (Unique to Imaging) |
|---|---|---|
| Image Preprocessing | oro.dicom, RNifti, imager | • Load medical imaging formats into R • Adjust intensity ranges & remove scanner artifacts • Convert pixel data into analyzable matrices |
| Segmentation & Region Detection | ANTsR, EBImage | • Isolate anatomical structures or lesions • Align images across timepoints or patients • Detect boundaries and highlight suspicious areas |
| Feature Extraction (Radiomics) | radiomics, caret, mlr3 | • Derive shape, texture & density measurements • Convert image regions into numerical descriptors • Prepare imaging features for predictive modeling |
| Predictive Modeling | randomForest, xgboost, glmnet | • Build classifiers to identify disease categories • Predict tumor progression or treatment response • Combine radiomic and clinical data for risk scoring |
| Visualization | ggplot2, plotly, rgl | • Generate 2D/3D rendering of segmented areas • Overlay detected regions on original scans • Create interactive imaging panels for clinicians |
| Reporting & Output | R Markdown, knitr, shiny | • Produce structured imaging summaries • Generate interactive radiology dashboards • Automate export of annotated scans & results |
| Case Insight: Medical Imaging for Early Tumor Detection Using R In a groundbreaking study, R was used to analyze MRI data for detecting early-stage brain tumors. Researchers employed ANTsR to process complex imaging data, highlighting irregularities such as tumors or plaques, particularly for Alzheimer’s disease. By automating the detection process, R significantly reduced the time spent analyzing each scan while improving accuracy. This R-powered approach is a game-changer, ensuring that tumors and diseases are identified at their earliest stages, where treatment can be most effective. Early diagnosis leads to better treatment options and improves long-term outcomes, showcasing the vital role of R in medical image analysis. |
5. Personalized Medicine
Every patient is different. Two people with the same diagnosis can respond very differently to the same drug. One recovers quickly; the other gets side effects or no benefit at all. Personalized medicine tries to understand why, by looking at a patient’s genes, medical history, lab markers, and even lifestyle factors to find the treatment that fits them best.
It’s basically moving from “What works for most people?” to “What works for this person?”
The Challenge Behind Personalization: Too Much Data, Too Many Contradictions
Before tools like R became common, personalization was more theory than practice. Doctors had patient history and lab results, but nothing that could combine genomics, biomarkers, symptoms, and long-term patterns into one meaningful picture.
The problems were straightforward:
- data came from different systems and didn’t match,
- genomic information was hard to interpret without proper statistics,
- small sample sizes made patterns easy to misread,
- and comparing treatment options objectively was almost impossible.
So even though the science existed, the practical workflow for real personalized care was missing.
R Programming in Personalized Medicine Changed the Game
R makes personalization achievable by turning scattered information into structured, analyzable insight.
With R, researchers and clinicians can bring all patient data (genomic variants, biomarkers, symptoms, treatment history, etc.) together and identify meaningful patterns that show why certain patients respond differently. R also helps them in predicting which therapy is likely to work best, visualize risks and expect outcomes clearly. Doctors could rely on R to produce patient-specific reports to make informed and confident decisions. Instead of guessing based on averages, R helps medical teams see evidence for each individual.
Why Life Science & Healthcare Students Should Care
This area is exploding. Pharma, oncology centers, genetic-testing companies, CROs, and research labs all need people who understand how to interpret patient-level data.
Learning how R fits into personalized medicine helps you:
- Understand how genes and clinical features connect
- Collaborate on precision-oncology or genomics projects
- Support doctors in making data-backed treatment decisions
- And work on the growing field of individualized therapies.
In short: Personalized medicine is the future of clinical care, and R is one of the tools turning that future into something practical.
R Programming Tools Used in Personalized Medicine & Treatment Planning
| Process Stage | R Tools / Packages | What the Tools Do (Unique Functions) |
|---|---|---|
| Data Integration | dplyr, tidyr, data.table | • Combine multi-source patient data into one profile • Match genomic records with clinical timelines • Align patient identifiers across datasets |
| Genomic & Biomarker Processing | Bioconductor, VariantAnnotation, GenomicRanges | • Extract mutation details linked to treatment choices • Annotate genetic variants with clinical relevance • Map biomarkers to disease-specific genomic regions |
| Predictive Modeling for Treatment Response | caret, randomForest, glmnet, xgboost | • Train models that estimate how well a patient will respond to therapies • Rank treatment options based on predicted effectiveness • Generate individualized risk or benefit scores |
| Risk Scoring & Outcome Estimation | survival, rms, mlr3 | • Produce personalized survival curves • Quantify relapse probabilities for specific treatments • Compare long-term outcomes for different therapy plans |
| Clinical Visualization | ggplot2, plotly, survminer | • Display patient-specific treatment comparison charts • Visualize genomic alterations tied to therapy decisions • Show survival probability curves tailored to individual patients |
| Reporting & Clinical Output | R Markdown, knitr, Shiny | • Create customized treatment recommendation documents • Build interactive clinician dashboards • Present patient-level analytics in an easy-to-read format |
| Case Insight: Oncological Treatment Planning with R In a study on personalized cancer treatment, oncologists used R to analyze genetic mutations, tumor markers, and patient history to develop targeted therapies for individuals. By employing machine learning models, they were able to predict how patients would respond to different chemotherapy regimens, ensuring that the treatment plan was customized to each patient’s genetic profile. This R-powered approach to personalized medicine is a game-changer, helping oncologists make more informed decisions and improve patient outcomes. With R, oncologists are not just treating the disease they’re tailoring treatment to the person, making cancer care more effective than ever before. |
Bioinformatics
Develop practical skills at the intersection of biology, data, and computation. This program prepares you to work with genomic and proteomic data, apply programming tools, and support real-world research and drug discovery workflows.

Duration: 12 months
Skills you’ll build:
Healthcare Cost-Effectiveness
Healthcare is full of tough choices. A new drug might extend life by a few months but cost far more than most hospitals or governments can realistically afford. Another treatment might be cheaper but offer very limited benefit. Cost-effectiveness analysis exists to answer a basic but uncomfortable question: Is the health benefit worth the cost?
This isn’t about cutting corners. It’s about making sure limited resources are used in ways that help the most people.
Before R: Important Questions, Slow Answers
Earlier, teams relied on spreadsheets and manual calculations to compare treatments. They had to pull together data from hospital bills, insurance claims, patient records, and clinical outcomes. Because this information came from different systems and used different formats, analysts spent more time fixing the data than actually studying it.
Even once the data was ready, running complex economic models was difficult. Predicting long-term costs, estimating quality-adjusted life years (QALYs), or testing how results change under different assumptions often pushed tools like Excel far beyond their limits. As a result, many decisions were delayed, or made with only a partial understanding of the real impact.
After R: Clear, Defensible Evidence for Policy Decisions
R changed this process by giving analysts a single environment where healthcare costs, patient outcomes, and long-term disease trends can all be studied together. Instead of wrestling with disconnected files, teams can clean and combine their data inside R, build models that realistically show how a disease progresses, and compare the true value of different treatments.
R also makes it easy to run large simulations that show best-case, worst-case, and most likely scenarios. This matters because healthcare decisions are rarely black-and-white. When R produces graphs and summaries showing how each treatment performs over time, policymakers finally get evidence they can trust and defend.
What once took months of manual work can now be repeated in minutes, with far greater clarity.
Why This Matters for Life Science and Healthcare Students
Every major healthcare system now uses cost-effectiveness studies to decide which treatments to fund, which vaccines to introduce, and how to allocate limited budgets. Pharma companies use these studies to demonstrate the value of new drugs. Governments use them to build fair and sustainable health programs. Hospitals use them to plan for long-term resource needs.
Students who understand how R fits into this process gain a major advantage. It helps them connect scientific outcomes with real-world health decisions, opening doors to roles in health economics, policy analysis, clinical research, pharmacoeconomics, and public-health planning. Even if someone never becomes a health economist, understanding how value is measured makes them a stronger and more aware healthcare professional.
R Programming Tools Used in Healthcare Cost-Effectiveness & Policy Analysis
| Process Stage | R Tools / Packages | What the Tools Do (Unique & Non-Repetitive) |
|---|---|---|
| Data Preparation & Standardization | dplyr, tidyr, data.table | • Organize cost data into economic models • Combine treatment, hospitalization, and insurance datasets • Align time periods and financial variables for comparison |
| Health Economics Modeling | BCEA (Bayesian Cost-Effectiveness Analysis), hesim, dampack | • Calculate ICERs (Incremental Cost-Effectiveness Ratios) • Run probabilistic sensitivity analyses (PSA) • Model lifetime costs and treatment benefits |
| Simulation & Scenario Testing | heemod, decisionSupport, markovchain | • Build Markov models for chronic conditions • Evaluate long-term treatment pathways and transitions • Test multiple policy scenarios (e.g., new vaccine rollouts) |
| Cost & Outcome Visualization | ggplot2, plotly, BCEA plotting tools | • Create cost-effectiveness planes (CE plane) • Generate cost-effectiveness acceptability curves (CEACs) • Visualize budget impact and threshold analyses |
| Policy Reporting & Decision Support | R Markdown, flexdashboard, Shiny | • Produce policy-ready economic evaluation reports • Build dashboards for exploring cost scenarios • Present models interactively for committees and stakeholders |
| Case Insight: Assessing the Cost-Effectiveness of New Healthcare Interventions Using R A recent study used R to assess the cost-effectiveness of a new vaccine for an emerging infectious disease. Using BCEA, researchers compared the costs of vaccination campaigns against the potential savings from reduced healthcare utilization, such as hospitalizations and treatments. The results showed that the vaccine would not only save lives but also reduce healthcare system burdens, making it a highly cost-effective intervention. R’s ability to provide these kinds of insights helps policymakers make more informed decisions, ensuring that healthcare systems can deliver the greatest value with their available resources. With R, the future of healthcare is not just about improving health outcomes but doing so in a way that is sustainable and economically efficient. |
7. Predicting Patient Outcomes in Chronic Disease
Chronic diseases like diabetes, heart failure, hypertension, or kidney disease don’t appear suddenly. They progress slowly, often showing small warning signs months before a major complication. Doctors already collect a lot of information from these patients, blood sugar trends, blood pressure readings, lab tests, medication history, even data from wearables. But seeing all these signals together, and understanding what they mean for the patient’s future, is extremely difficult without the right tools.
This is where predictive analytics comes in: it helps answer questions like “Is this patient headed toward a hospitalization?” or “Who needs urgent intervention?” long before symptoms become dangerous.
Before R: Valuable Data, But No Way to See the Full Picture
For years, clinicians had access to these records, but the data lived in different systems and formats. One piece was in the EHR, another in lab reports, another in patient diaries, and another in wearable apps. Even when all the data was available, it was nearly impossible to combine it into a timeline that showed how the patient was actually progressing.
It was hard to identify patterns from noise, and predicting risks relied mostly on experience, not evidence. Without a structured way to analyze long-term data, many complications were detected only when they had already become serious.
After R: Clear Health Trajectories and Early Intervention
R helps turn years of scattered patient information into meaningful timelines that show how someone’s health is changing. Once the data is organized, R can pick up subtle trends, a slow rise in blood pressure, irregular heart-rate patterns, unstable glucose swings, or gradual kidney decline, long before they trigger a medical emergency.
By building prediction models, R estimates how likely a patient is to experience events like hospitalization, stroke, or sudden worsening of symptoms. And instead of burying this in numbers, R generates risk curves and simple visual summaries that clinicians can read instantly. This allows doctors to adjust treatment plans earlier, prevent complications, and personalize long-term care.
Instead of reacting to problems, healthcare teams can stay one step ahead.
Why This Matters for Life Science and Healthcare Students
Chronic diseases make up a huge portion of global healthcare needs, and every hospital, insurance company, and public-health agency now relies on predictive analytics to manage them. Understanding how R supports this work helps students see how data and biology connect in real-world care. It opens opportunities in clinical research, digital health, chronic-disease management programs, wearable-device analytics, and health-tech companies building early-warning systems.
Most importantly, it shows future healthcare professionals how data, when used correctly, can transform patient care from reactive to preventive, a shift that defines the future of medicine.
R Programming Tools Used in Predicting Chronic Disease Outcomes
| Process Stage | R Tools / Packages | What the Tools Do |
|---|---|---|
| Data Cleaning & Time-Series Structuring | dplyr, zoo, lubridate | • Organize long-term health data into timelines • Handle irregular timestamps, missing dates, and noisy readings • Standardize clinical measurements across visits |
| Feature Engineering for Clinical Predictors | caret, recipes, tsfeatures | • Create clinically meaningful variables (e.g., glucose variability, BP trend slopes) • Normalize health indicators for modeling • Extract temporal features from wearable or sensor data |
| Risk Modeling & Prediction | randomForest, xgboost, glmnet | • Predict complications (stroke, hospitalization, kidney failure) • Rank the most important predictors for each patient • Build models tailored for chronic disease progression |
| Trend Visualization & Risk Trajectories | ggplot2, plotly, timetk | • Draw patient-specific risk curves over time • Visualize changes in vitals, labs, and symptoms • Build interactive time-series charts for clinicians |
| Clinical Reporting & Monitoring Dashboards | R Markdown, flexdashboard, Shiny | • Generate clinician-friendly reports showing risk levels • Provide interactive dashboards for ongoing monitoring • Enable early alert systems for high-risk patients |
| Case Insight: Predicting Heart Disease Risk in Diabetic Patients Using R In a recent study, R was used to predict the risk of heart attacks and strokes in diabetic patients. Using randomForest and glmnet, researchers built a predictive model based on factors like blood sugar levels, cholesterol, and physical activity. The model successfully identified high-risk patients who could benefit from early interventions, like lifestyle changes or medication adjustments. This R-powered approach is revolutionizing how chronic diseases are managed by providing more accurate, data-driven predictions that guide clinical decisions and improve patient care. By focusing on early risk identification, healthcare providers can take timely action, helping prevent serious complications and ensuring better health outcomes. |
8. Health Informatics & Data Integration
In a hospital, a single patient’s information lives in many different systems. Lab tests sit in one database, imaging files in another, prescriptions and pharmacy logs somewhere else, and wearable-device data inside its own separate platforms. All of these pieces matter for care, yet they rarely connect smoothly. Health informatics tries to bring them together so doctors and administrators can finally see a complete, accurate picture of the patient. But because each system uses different formats and codes, the process is harder than it sounds.
Before R: A Lot of Data, But No Unified View
Traditionally, teams tried to merge this information manually. They downloaded spreadsheets, copied values from hospital systems, and tried to line things up patient by patient. But even small mismatches in names, dates, or codes made merging difficult. Records didn’t align naturally, timestamps varied across systems, and imaging files needed special tools to even open. The result was that hospitals technically had a lot of data, yet lacked a single source of truth. Important trends stayed hidden, workflow delays were hard to trace, and clinicians often made decisions based on incomplete information.
After R Programming in Healthcare Data Analytics: A Clean, Connected Picture of Patient Journeys
R finally gives analysts a way to bring all these pieces together. Once the different datasets are imported, R can clean them, standardize formats, fix inconsistencies, match patient identifiers, and align timelines. What used to be scattered becomes a unified patient story. When the data is organized this way, patterns begin to appear clearly, how long diagnoses take, where treatment delays happen, which processes slow down patient care, and what parts of the hospital system need improvement.
R doesn’t stop at cleaning. It also turns these insights into visual dashboards and clear summaries that teams can use immediately. Clinicians see patient journeys more clearly, administrators understand bottlenecks, and hospitals make decisions based on complete and reliable information instead of fragmented data.
Why This Matters to Life Science and Healthcare Students
Healthcare is becoming more data-driven every year, and understanding how information flows through a hospital system is now a core skill. Students who learn how R fits into health informatics gain a strong advantage. They develop the ability to interpret patient data in a broader context—biological, clinical, and operational. This opens the door to careers in clinical analytics, hospital quality teams, digital health companies, EHR-driven projects, and research environments where integrated data is essential.
Seeing the full patient story in one place is powerful, and R is one of the tools making that possible.
| Process Stage | R Tools / Packages | What the Tools Do |
|---|---|---|
| Data Extraction & Cleaning | dplyr, data.table, janitor | • Clean EHR tables and remove coding inconsistencies • Handle large administrative datasets efficiently • Standardize variable names and fix metadata issues |
| Health Data Integration & Mapping | tidyverse, FHIR, jsonlite | • Merge patient records from multiple clinical systems • Work with FHIR-formatted data for healthcare interoperability • Parse and combine JSON-based EHR or wearable data |
| Clinical & Operational Analysis | tableone, healthcareai, arules | • Generate clinical summary tables for patient cohorts • Detect workflow inefficiencies or risk patterns • Identify associations in patient behavior or treatment pathways |
| Visualization of Integrated Data | ggplot2, plotly, visNetwork | • Visualize hospital workflows, patient journeys, and diagnostic timelines • Build interactive charts for care-coordination teams • Map connections between patient records or clinical events |
| Dashboards & Reporting | Shiny, flexdashboard, R Markdown | • Create real-time hospital dashboards for monitoring patient status • Build administrative dashboards for admissions, labs, or resource allocation • Generate structured reports for clinical leadership |
| Case Insight: Comprehensive Patient Profiling Using R A hospital system recently implemented R to integrate data from EHRs, wearable devices, and lab results to create a comprehensive patient profile. Using dplyr and tidyr, they merged data from various sources into a single dataset, Which enabled healthcare professionals to track patient progress over time more effectively. By having a full, real-time picture of the patient’s health, clinicians were able to adjust treatments more quickly and prevent complications, leading to better overall care. This integration of health data with R has proven to be a game-changer in how healthcare providers make decisions, ensuring that patients receive timely, personalized care and improving the overall efficiency of the healthcare system. |
Career Opportunities After Learning R Programming in Healthcare
As healthcare data grows, R programming is becoming essential in fields like AI, machine learning, bioinformatics, and genomics. R’s strengths in real-time data processing and predictive analytics are driving innovations in personalized care and clinical decision making, making it an indispensable tool for professionals. Careers leveraging R include healthcare data science, clinical data analysis, and bioinformatics, where professionals analyze data and develop predictive models. These roles increasingly rely on R for health data science, where professionals combine statistical rigor with real-world clinical datasets to drive insights.
For students entering healthcare, R programming unlocks access to high demand roles. It’s not just about mastering the language, but how students position themselves. Focusing on real-world projects and gaining hands-on experience through internships and open-source projects allows students to build a strong portfolio and network with industry professionals.
As demand for healthcare data professionals grows, salaries are rising. In India, data scientist roles typically offer ₹6 LPA – ₹14.4 LPA, while in the U.S., the average salary is US $129,336/yr. with the growing focus on personalized medicine and AI/ML, the demand for R programming skills is expected to rise, offering abundant opportunities for professionals and students to shape healthcare’s future.
Conclusion
What makes R valuable is not the language itself, but what it enables. It allows healthcare professionals to work with messy, high-volume data, apply the right statistical methods, and produce results that can be trusted, reviewed, and reused. This is why R continues to be used across hospitals, pharma companies, research labs, and public-health organizations worldwide.
For students and early professionals, learning R means moving beyond theory. It means understanding how data supports drug development, disease monitoring, patient safety, and healthcare policy in real-world settings. As healthcare becomes increasingly data-driven, professionals who can analyze, interpret, and clearly communicate insights using R will remain in strong demand.
Building these skills requires more than isolated tutorials. It requires structured learning, real datasets, and domain-specific context—at CliniLaunch that’s exactly what our career-focused healthcare and life sciences programs aim to provide. If you’re looking to grow into roles where data genuinely shapes healthcare decisions, exploring the right learning path early makes all the difference.
FAQs
1. How is R programming used in healthcare?
R is used to analyze clinical data, run statistical tests, model disease trends, study genomics, and support research in trials, epidemiology, and public health.
2. Can I use R instead of SPSS?
Yes. R can do everything SPSS does and more. It’s widely used in research because it’s flexible, transparent, and free.
3. Which language is best for medical coding?
Medical coding itself doesn’t require programming.
For analytics and healthcare data work, R and Python are more relevant than coding languages used in billing systems.
4. Can R read SPSS files?
Yes. R can easily import SPSS files using packages like haven.
5. Can I learn R in 3 months?
Yes, for practical healthcare use. You can learn data handling, visualization, and basic analysis in 3 months with focused practice.
6. How do I import data into R?
You can import data from Excel, CSV, SPSS, databases, and APIs using built-in functions and packages like readr, readxl, and haven.
7. Is R harder than Excel?
Yes, initially. But R is far more powerful once you move beyond basic analysis and repetitive manual work.
8. Do epidemiologists use R?
Yes. R is one of the most widely used tools in epidemiology for outbreak analysis, modeling, forecasting, and reporting.
9. Which programming language is best for bioinformatics?
R and Python are the top choices. R is especially strong in statistics, genomics, and biological data analysis.
10. What is R used for in biology?
R is used to analyze gene expression, genomic data, experimental results, and biological trends in research and healthcare.





